(Feng Mok) 7 Tips To Manage Your Child’s Hives
Concerned about feng mok (also known as fong mok or fung mok)?
Since childhood, we call these rashes by other names too like “ruam”.
Your child has been well all and suddenly, you see big patches of red rashes appearing on the face and body.
Otherwise, your child appears alright apart from the frequent scratching because of the itchiness.
What is feng mok?
Feng mok could be an allergic reaction.
At least that is what most parents would think, the very first thing that crosses their minds.
It is possible but not all the time.
In this topic, we will touch on these:
- what hives look like
- the causes of hives/feng mok/ruam
- what to do with hives
- treatment for hives

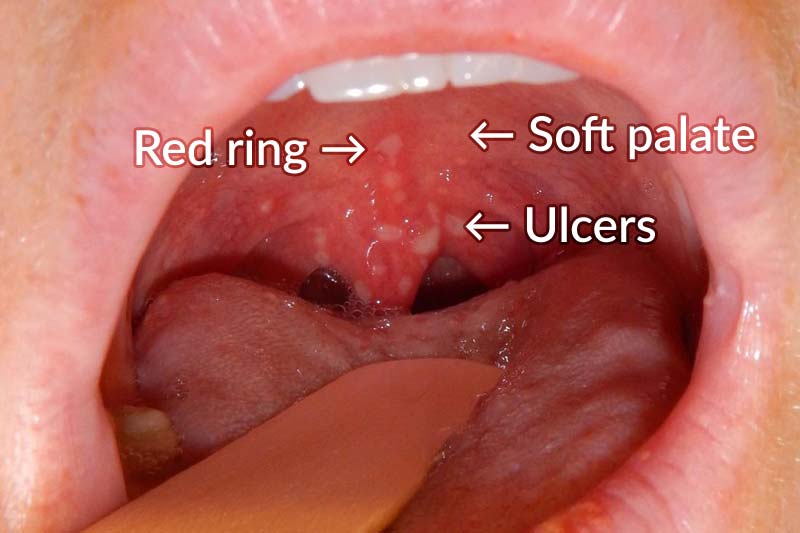
Feng mok appears as red large patches of rash on the body.
Hives are bumpy red rashes that appear on the skin which is itchy most of the time, although sometimes hives can be painful too.
They look like big scratch marks too at times.
They look like mosquito bites, just that they appear bigger and redder.
They can appear anywhere on the body, be it the face, body or limbs.
As fast as they appear, they disappear very fast too.

A child will scratch regardless of what you tell them.
What causes hives?
One of the more common reasons hives appear is an allergic reaction towards a certain type of food or medication.
Or even after being bitten by an insect.
The common food types include:
- berries
- egg
- milk
- nuts
- wheat

Food that may trigger an allergy.
Hives can also appear in non-allergic conditions such as:
- change in temperature
- exercise
- stress or anxiety
- infections
However, a majority of the time, you will not be able to find out the exact cause.

Antihistamines help to relieve hives.
7 tips to treat hives
Most hives in children go away spontaneously even without medications, sometimes within a matter of hours.
If it troubles your child, these are what you can do:
Stay out of the sun
Direct contact with the sun for a long period of time can actually trigger hives.
Try to get your child to stay in a cool environment, which will reduce the incidence of getting hives.
Stress-free environment
If your child is highly stressed out, it actually increases the risk of hives developing.
Try to keep home as calm as possible.
Excessive homework, arguments, parenting methods, etc. should be dealt with more carefully.
Use antihistamines
If you are familiar with runny nose medications, those are called antihistamines.
Hives occur when there are high levels of histamine are released into the skin.
Histamine is a chemical compound released by our cells in response to allergies or injuries.
In order to counteract with the reaction, antihistamines are helpful in this context.

A child taking in medication.
Some of the antihistamines that you can use:
- Cetirizine (Zyrtec)
- Desloratadine (Aerius)
- Chlorphenamine (Piriton)
These medications mentioned above are generally safe to be used for children above 2 years of age.
It relieves the itchiness from hives and prevents further recurrence.
Also, it can be used as a runny nose medication as well.
You can purchase these medications over the counter from the pharmacy.
Just be sure to get the right dose by reading the instructions or from the pharmacist in-charged before giving it to your child.
Take a cool bath
A cool shower helps to reduce the itchiness and chances of hives forming.
Similarly, you can also use a cold towel to wrap over the itchy areas.
Or, you can use ice packs wrapped in a towel and compress it over itchy areas for a couple of minutes.
Calamine lotion
If you’ve had chickenpox before, you may come across calamine lotion.
It is a cool lotion which is dry after application and has a cooling effect over the skin.
It helps to reduce itchiness and lower the chances of scratching.
Moisturising cream
Somewhat similar to calamine lotion, moisturising cream keeps the skin moist instead of dry.
A moisturising cream with anti-itch properties such as Suu Balm Kids helps to reduce itchiness almost instantly.
It contains 1% methol, made directly from mint leaves which helps to relieve itching really fast.
Steroidal cream
As you probably know, most parents hate it.
Even the mention of steroids strikes fear in most parents.
However, if steroidal cream is used appropriately, it can actually improve the outcome.
Using a low dose of steroidal cream such as 1% hydrocortisone is helpful in managing hives.

Skin allergy test.
Is an allergy test necessary?
A lot of parents have been asking countless times whether their child needs an allergy testing.
Should your child be doing one too?
The answer is yes, and also a no.
A majority of the time, it is no. If you have the read the above, you will not be able to identify the cause of hives.
Even if you can do an allergy test, it will not be able to pinpoint the exact cause.
So when is an allergy test useful?
An allergy test should be performed if there is a bad allergic reaction.
Meaning, if a child has difficulty in breathing upon getting hives or gets a bad swelling because of it, then it will be useful to do one.
At least with the results, you can try to avoid certain foods or products.
Like I said earlier, it may not tell you the cause of the hives, but at least you can avoid the items that can trigger an allergic reaction.

Hives caused by insect bites.
When do hives require medical attention?
Here’s a short article from PubMed (a medical portal for research papers).
“In children, urticaria is more often acute than chronic. Acute urticaria is caused frequently by IgE-mediated allergic reactions to foods or by acute infections, usually viral respiratory tract infections.”
“Approximately 30% of children with chronic urticaria have a positive ASST and approximately 4% have positive thyroid peroxidase antibodies.“
“Referral to a specialist centre is suggested if the child has very severe symptoms.“

The appearance of a hive.
Now, don’t worry about all the bombastic words above. Here’s what it means:
- Hives are part of the big group called urticaria.
- Hives in children are usually caused by a known/unknown triggering factor which should go away over time.
- Chronic refers to hives that are stubborn, that keeps happening again and again.
- If it is chronic, your child should seek medical attention as there may be other underlying health conditions rather than just simply hives.
- Severe symptoms include difficulty in breathing, coughing badly or there is significant swelling of the skin, apart from the rashes.
In summary, most hives do not require further workup unless other symptoms such as above present.
Hopefully, you know what to do now if your child gets it.
Do you have a child with hives?
What are the ways you use to combat it?
Share your thoughts and leave us a comment below!
References:
- An approach to the patient with urticaria | PubMed
- Hives (Children) | WebMD
- Hives | HealthChildren.org by American Academy of Pediatrics